The following letter was submitted on behalf of AHQA’s members as part of the comment period for the MACRA Proposed Rule. To download a PDF version of this letter, click here.
Andrew M. Slavitt, Acting Administrator
Centers for Medicare & Medicaid Services (CMS)
U.S. Department of Health and Human Services
Attention: CMS-5517-P
P.O. Box 8013
Baltimore, MD 21244-8013
Dear Acting Administrator Slavitt:
Thank you for the opportunity to comment on the proposed rules for Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive Under the Physician Fee Schedule, and Criteria for Physician Focused Payment Models.
Our organization, the American Health Quality Association (AHQA), represents the Quality Innovation Network-Quality Improvement Organizations (QIN-QIOs) and their quality improvement partners throughout the United States, Puerto Rico, the Virgin Islands, and the outer Pacific islands. Our association’s goal is to make health care better, safer, and available at a lower cost.
As Medicare-funded organizations charged with working with providers, beneficiaries, families, and stakeholders to improve quality for our nation’s seniors, QIN-QIOs are keenly interested in the provisions of the proposed rule. We strongly support the core principles outlined in the Notice of Proposed Rule Making (NPRM) of simplification and reduction of administrative burden for clinicians and providers. We endorse the effort by CMS to reduce the payment compliance burden for providers without sacrificing the goal of improving outcomes for patients and families.
Below are our comments regarding each of the four performance categories within the NPRM.
QUALITY DOMAIN
We urge CMS to design and make widely available a self-assessment tool that would permit providers to assess their performance against the quality measures benchmarks CMS intends to publish on a routine basis. It is imperative that eligible providers be offered the opportunity to gauge their performance on the quality measures well ahead of the deadline for data submission so that they may have the chance to make any necessary adjustments to improve their performance. In a similar fashion, CMS should encourage Electronic Health Records (her) vendors to provide the functionality needed for providers to easily access the data to evaluate their performance against the MIPS quality domain measures on an ongoing basis.
In addition, we encourage CMS to leverage its network of QIN-QIOs to assist providers in using the self-assessment tool to determine performance against the MIPS standards, and offer providers technical assistance to address performance shortcomings. QIN-QIOs have worked for more than a decade supporting clinicians in reporting quality data (PQRS, etc.) to CMS and have worked with providers to redesign care practices and workflow to improve performance on quality metrics.
We urge CMS to review the approach it intends to take in scoring “topped out” quality measures. The determination of whether a provider should or should not receive maximum credit for achieving 100% compliance on a performance measure should not be predicated on the number of colleagues reaching a similar level of achievement. Such an approach sends the wrong message to providers, inasmuch as it implies that performance measure excellence is the product of the number of providers attaining such a high level of performance, rather than the performance of any one provider.
We suggest that CMS consider adjusting the scoring methodology under this domain to recognize year-over-year performance improvement on each of the quality measures. CMS has substantial experience designing quality measurement programs that recognize absolute performance as well as relative improvement. We believe a similar, two-prong scoring approach to the MIPS quality domain scoring, starting in Year 2 of the program, makes the most sense.
We strongly encourage CMS to consider keeping the set of MIPS quality domain measures the same for a two- to three-year period and that the agency require and/or offer incentives to providers to report on the same measures for more than one year. Since quality improvement interventions usually take more than a single year to take hold and result in actual performance change, the opportunity to report on the same set of quality measures for more than one year (year over year) would allow providers the opportunity to focus on making meaningful improvements to the quality of care they deliver to their patients.
RESOURCE USE
We encourage CMS to reconsider the use of a minimum sample size of 20 for calculating the resource use measures. While we understand that reducing the sample size from 125 (under the Value-Based Payment Modifier (VBPM) program) to 20 is intended to increase the number of qualifying resource use measure calculations for the program, the literature on quality and resource use measures has consistently shown the need to use sample sizes of no smaller than 100 in most cases for measures calculation to achieve statistical stability. Given the financial consequences surrounding the MIPS program, we suggest that CMS reconsider the minimum sample size to qualify a provider for an episode of care measure under the resource use domain.
As noted above in the Quality Domain performance category, we suggest that CMS consider adjusting the scoring methodology under this domain to recognize year-over-year performance improvement on each of the quality measures. We reiterate that CMS has substantial experience designing quality measurement programs that recognize absolute performance as well as relative improvement. We believe a similar, two-prong scoring approach to the MIPS resource use scoring, starting in Year 2 of the program, makes the most sense.
We are concerned about physicians and providers who do not have access to a health information exchange. In these cases, we recommend a hardship exemption option for this objective.
Since the EHR Incentive program still exists for Medicaid providers, it is unclear if the EHR vendors will be required to provide two sets of reports (one for each program). We recommend aligning Medicaid EHR Incentives and Medicare MIPS quickly, as well as requiring EHR vendors to submit quality measures and attestations for all three MIPS categories—Quality, Advancing Care Information (ACI), and Clinical Practice Improvement Activities (CPIA).
We also suggest incorporating some increased value, via bonus points, for EHR reporting. Certainly, one of the goals with the EHR incentive program was to build, design, and maintain systems which capture important data points for quality measurement in a consistent, structured manner. Increasing the value of reporting via the EHR reporting method encourages clinicians to use their EHR systems in a manner to promote better visibility and granularity with quality data, as well as urges EHR vendors to make this functionality more available and streamlined to gather, track, and trend quality data. Expending multiple hours to extract or abstract data is an inefficient use of time and materials and diverts clinicians away from improvement activities.
The MIPS rule specifies that MIPS-eligible clinicians submitting data for the ACI category are required to collect data from all locations where they provide service and aggregate the data for these measures. Requiring information from all practices locations across TINs is an unnecessary burden which can be eliminated as it serves no useful purpose. We recommend that the same process currently utilized for PQRS be adopted for MIPS, allowing for a TIN/NPI combination for reporting for all three MIPS categories. In this way, each clinic will be responsible for reporting for all NPIs that perform services at their clinics.
Multiple mechanisms are available for providers to submit their quality measures, ACI, and CPIA. We recommend streamlining the submission process for all categories, whether a measure or attestation, using the same standardized format. For example, EHR vendors, registries, and QCDRs would be required to use the same QRDA I or III format to streamline submission of all three categories of MIPS.
We recommend reducing the number of Electronic Clinical Quality Measures (eCQM) revisions per year. Current experience shows the EHR vendors often cannot or do not update the software and reports in enough time for providers to accurately monitor their measures to ensure success. The reality of time delays, based on updates, handoffs and system upgrades needs to be recognized.
Additionally, we ask that CMS consider eliminating the various requirements pertaining to the different reporting mechanisms. We urge that CMS make the eCQM specifications (found on eqi.healthit.gov) the baseline specifications, regardless of the reporting mechanism. We recommend that CMS not change volume requirements based on which mechanism is utilized for reporting purposes. The only difference should pertain to whether practices include all encounters or only Medicare FFS encounters.
CPIA Domain
The relatively low weighting of CPIA (15% of the total score in Year 1) would seem to undercut the goal of actively encouraging providers to commit to the infrastructure necessary to achieve long-term success. The broad emphasis on care coordination, beneficiary engagement, and patient safety is appropriate, but we believe CMS should include a fourth category that allows practices to focus on office efficiency/operations.
The program currently identifies an annual update to the list of approved activities. While this is a realistic timeframe for revisions, it is important to recognize that practices are likely to develop multi-year improvement strategies and the sudden removal of an approved activity could undermine program stability. For this reason, it is important that topics identified for termination should be allowed to continue for one year beyond initial notification to allow for sufficient notice to participating practices.
While the flexibility of an “a la carte” approach to obtaining CPIA points is sensible, it is important that CPIA efforts be tied to the areas where providers are struggling. Experience has shown that physicians are more likely to participate in programs in areas where they feel confident in their skills, as opposed to areas where they may be struggling or have limited experience. We believe a long-term goal of the CPIA program should be to target Clinical Practice Improvement Activities to identified practice deficiencies.
Given the broad portfolio of individual projects within the QIN-QIOs, we believe that individual credit should be provided for each QIO project that a provider participates in and not simply a uniform point(s) award for any participation.
While we applaud the emphasis on Patient-Centered Medical Home (PCMH) models within the CPIA, it is our understanding that the majority of certification programs do not have a requirement for ongoing, active clinical improvement efforts. AHQA strongly recommends a flexible approach to quality assessment that emphasizes outcomes of care and that favors continuous quality improvement methodologies rather than rigid, process-oriented certification models. Relying on certification as a means of quality assessment runs the risk of practices checking off items but leaving the way they operate intact and not actually realigning efforts to produce higher quality and more cost effective care.
While recognition as a PCMH provides full credit for CPIA to practices, this certification is not an option for many of the specialty physicians that are likewise affected by the Quality Payment Program (QPP). As such, we recommend that the rulemaking process be used to also allow full credit for specialty practices receiving PCMH Specialty Practice Recognition.
We note that “non-patient facing” providers can perform a single activity, instead of having to meet full requirements. We are concerned that this exception implies a lesser need for quality improvement within these practices. We maintain that Clinical Performance Improvement Activities are equally valuable for all medical specialties and that all providers should be held to the same standard.
The rationale for CPIA half credit for participation in Advanced Alternative Payment Models (APMs) is unclear, in light of the full credit for PCMH participation. Success in APMs is dependent upon CPIA and therefore we believe that full credit should be extended to practices participating in those models as well.
Although potentially blurring the lines of the point categories, we believe that it is valuable to recognize those quality improvement efforts that have not yet been formally adopted by the program. To recognize these innovative efforts, we propose that an improvement threshold be set for quality measures and that attainment of this level of improvement be considered evidence of CPIA and rewarded with CPIA points.
We recognize the value of a broad approach to improvement, but believe that many efforts require a multi-year approach. For this reason, we propose that individual topics may be pursued by an individual provider for up to three years, but that following this period, providers be required to select a different area of focus.
Given the aggregated data model for physicians with multi-site practices, it isn’t clear how this issue is to be handled regarding CPIA. Due to the significant effort required at each site and the general lack of “economy of scale” for quality improvement efforts across multiple practice locations, we believe that a provider should be allowed to receive points for each site in which they are participating.
An early introduction of the CPIA program, prior to the 2019 rollout of the remainder of the project, could serve to “ramp-up” efforts that allow practices to build the infrastructure needed for their eventual success and allow a low-risk, phasing-in approach to the scoring aspects of the QPP.
As part of efforts aimed at administrative simplification, we believe that a valuable service could be presented by QIN-QIOs through their direct reporting of participating providers’ CPIA activities.
One way to align quality improvement expertise provided to practices across the nation would be for MIPS support contractors to rely on the same elements of practice transformation that are being rolled out in the Transforming Clinical Practice Initiative (TCPI). Under this scenario, MIPS support would focus on the five phases and milestones being utilized for TCPI in primary and specialty care. These consist of: Phase 1 (aim setting/capacity building), Phase 2 (reporting and using data to improve quality), Phase 3 (achieving lower costs, better care, and better health), Phase 4 (getting to benchmark status), and Phase 5 (demonstrating sustained capability to generate better care and better health at lower cost).
Advancing Care Information (ACI)
We applaud efforts to advance the exchange of health care information. We have concerns that the interoperability requirements permitting exchange of clinical messages with providers using another EHR system will prove to be quite costly. We strongly recommend that interoperability costs be the responsibility of the EHR vendors. There are many instances in which one provider sends a Creditable Coverage Disclosure (CCD) to another provider with another system, but the receiving system cannot open it. The Comprehensive Primary Care plus (CPC+) model requires that the EHR vendors meet the necessary requirements at no additional cost. This model should be applied for MIPS.
If the Office of the National Coordinator for Health Information Technology (ONC) authorized bodies find that a provider is unable to open a CCD from another provider with a different EHR, the penalty should be assigned to the EHR Vendor as opposed to the provider. Indeed, it is our understanding that some EHR vendors are using their own version of CCDs, which render them unusable by other EHR vendors.
Additionally, the rule needs to provide clarification on when eligible hospitals must also be compliant with Stage 3 ACI-like measures, insofar as many of them attested to both Medicare and Medicaid. Physicians and hospitals need to be able to communicate effectively for physicians to be successful regarding this measure.
We anticipate security to be the biggest risk in the MIPS ACI requirements. Physicians still do not have an accurate understanding of what is required in a risk analysis, and it appears that few rural, small, or solo physician practices have conducted full analyses. We recommend continuing education on this topic.
Supplemental Information
Suggested Educational Resource
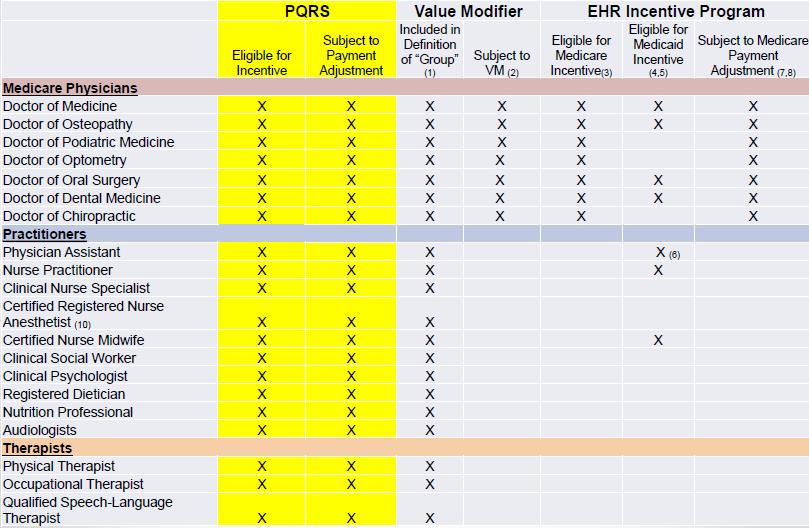
There has been discussion amongst the QIN-QIOs about who is considered/qualifies as an eligible clinician and for which categories. We have found that visual displays outlining which providers are subject to which categories of MIPS (such as in the table below) offer clear, concise guidance, are well received by providers, and help to eliminate confusion. We recommend that CMS utilize this table or a similar tool to aid in communication and education efforts around the payment models.
Rural Health Centers (RHCs) and Federal Qualified Health Centers (FQHCs)
Services billed under RHCs/FQHCs are currently exempt from Physician Quality Reporting System (PQRS) and Value Modifier. This exemption has provided necessary shelter for these programs and prevented them from expending valuable resources attempting to meet criteria for multiple quality programs during the same timeframe. We support the proposal to exclude RHCs/FQHCs from the MIPS all-inclusive payment rate.
Rural Health Centers (RHCs) and Critical Access Hospitals (CAHs)
Presently, some providers offering services at RHCs also provide Medicare Part B Physician Free Schedule (PFS) services which are subjected to PQRS. An example would be providing services in a Critical Access Hospital (CAH) such as emergency medicine and outpatient procedures. The Certified EHR Technology (CEHRT) in the CAH is not configured to give accessibility to electronic Clinical Quality Measures for eligible clinicians as the hospital CEHRT is designed to provide electronic Clinical Quality Measures mapped to the Hospital Inpatient Quality Reporting (HIQR) measures rather than the PQRS measures. The eligible clinicians typically have a greater patient volume in the clinic as well as an increased ability to effect positive change in quality measures in the clinic. In the above scenario, quality measures for eligible clinicians are required from the CAH, where they see fewer patients, have less ability to impact change, and must extract measurement data manually. Substantial resources are being spent gathering data rather than implementing improvement programs.
Our recommendation is to allow providers in a CAH to submit data to MIPS for all appropriate categories from the RHC setting in lieu of submitting data from only the setting in which the Medicare Part B PFS claims are submitted.
Thank you for the greatly appreciated opportunity to comment on the proposed rule for the Quality Payment Program and the MIPs or APM paths. We believe our observations, comments, and recommendations are aligned with and in support of CMS and Congresses’ intent with MACRA, as well as the long history and demonstrated successes of the QIN-QIOS in partnering with CMS to achieve substantive improvement in health care quality.
Regards,
Colleen Delaney Eubanks, CAE
Executive Director
